In this exploration, we delve into the fascinating connection between Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and the intricate world of the human gut microbiome.
What is the link between these functional gastrointestinal disorders and the microbiome? How does the microbiome and gut flora contribute to the development, management, and treatment of IBS and IBD? Can microbial insights help us treat IBS patients and manage IBS symptoms?
This article will dive into these topics and more. But first, to answer these questions, we need to understand what IBS and IBD are.
Introduction: Irritable Bowel Syndrome
IBS is a common gastrointestinal disorder affecting around 10-15% of the global population. Predominant irritable bowel syndrome symptoms include abdominal pain or discomfort, bloating, a change in gut motility, altered bowel habits (diarrhea and constipation), without any apparent underlying structural or biochemical cause.
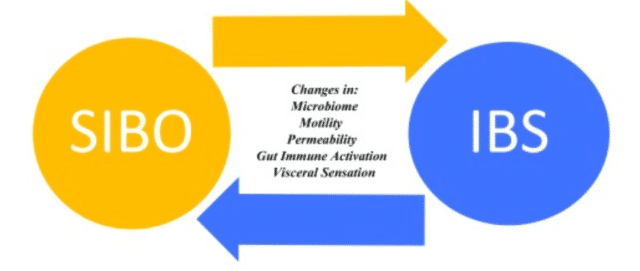
While the exact cause of IBS is still unknown, studies have shown a strong association between alterations or overgrowth in intestinal bacteria in the gut microbiome and IBS patients.
Research has demonstrated IBS patients to have an imbalance in their gut microbiota composition, known as dysbiosis, compared to healthy individuals. This disruption in the gut microbiome can lead to increased intestinal permeability, inflammation, and altered immune responses, all of which can contribute to IBS symptoms.
This creates a new question for researchers to answer—is small intestinal bacterial overgrowth the chicken or the egg?
Introduction: Inflammatory Bowel Disease
In contrast to IBS, IBD is a group of chronic inflammatory conditions affecting the digestive tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. While the exact cause of IBD is still unknown, research suggests that an individual’s genetic makeup and environmental factors play a role in its development.
However, recent studies have also shown a strong association between IBD and alterations in the gut microbiome. Frontiers research states:
A large number of studies have investigated the relationship between the genetic factors related to the susceptibility to IBD and the gut microbiota of patients by using high-throughput sequencing. IBD is considered the outcome of the interaction between host and microorganisms, including intestinal microbial factors, abnormal immune response, and a damaged intestinal mucosal barrier.
Unravelling the Microbial Tapestry in IBD & IBS: Microbiome Connection
When we shift our focus to patients with IBS or other inflammatory bowel diseases, we can see an abundance of correlation to the complex tapestry of the gut microbiome. In the sections below, we’ll explore the key players when it comes to the IBS/microbiome connection, through a handy analogy to help aid understanding.
Gut Microbiota Composition and the Enteric Nervous System
Imagine the gut as a bustling metropolis, with gut microbes being the citizens of this city. In the city’s day-to-day functioning, the enteric nervous system acts as the communication network, transmitting information across different regions. This network ensures the city functions smoothly, from managing transportation to overseeing public health.
Just as the city’s infrastructure would falter if the communication network breaks down, so does the gut when the enteric nervous system is compromised, leading to conditions like IBS.
Intestinal Inflammation & the Immune System
Now, consider intestinal inflammation or mucosal inflammation as a wildfire breaking out in the city. This fire affects the city’s inhabitants (the microbes) and disrupts the normal functioning. This can lead to the dysfunction of intestinal epithelial cells, and an increase in pathogenic bacteria.
The immune activation can be equated to the city’s fire department, trying to control and extinguish the inflammation. But, if the fire department is overzealous and damages parts of the city or if it fails to quench the fire (pathogenic bacteria) adequately, it leads to persistent issues.
Short-Chain Fatty Acids
Lastly, Short Chain Fatty Acids (SCFAs) can be likened to the city’s energy supply. They are the primary energy source for colon cells and are crucial in maintaining the health and integrity of the gut lining.
When the city’s energy supply is disrupted, the city experiences blackouts and breakdowns, much like how the gut behaves when SCFAs levels are imbalanced. In this urban jungle of the gut, every element is interlinked, and any disruption can lead to issues like IBS playing out on this microcosmic stage.
How the Gut Microbiome Can Support IBS Management
As we have explored, the gut microbiome can both support treatment of, and potentially play a part in the development of IBS. But, with this newfound understanding of the microbiome’s role in our digestive health, can we use it to help manage or even prevent IBS?
Diet & Lifestyle Changes (Prebiotics & Probiotics)
Evidence suggests that dietary and lifestyle changes can improve symptoms of IBS by modulating the gut microbiome composition and reducing inflammation. Including probiotic-rich foods, fiber-rich vegetables, and limiting processed foods and alcohol may help establish a healthy balance in the gut microbiome.
Another avenue being explored in managing IBS through the gut microbiome is prebiotic and probiotic interventions. While probiotics refer to live beneficial microbes, prebiotics are food sources that promote the growth of these beneficial bacteria.
Fecal Microbiota Transplantation (FMT)
In the quest to restore balance in the gut microbiome, Fecal Microbiota Transplantation (FMT) emerges as a fascinating avenue. Imagine FMT as a replenishing of the citizens of your gut, introducing a harmonious blend of beneficial microbes from a healthy donor to reset the gut microbiota composition.
This procedure, though still under scrutiny, holds promise in alleviating symptoms of patients with IBS in certain cases. It can also be coupled with lifestyle and dietary modifications to strengthen the gut microbiome’s resilience.
Review and Meta-Analysis
To navigate the scientific waters surrounding IBS, IBD, and the microbiome, researchers often conduct systematic review and meta-analyses. These comprehensive analyses sift through a plethora of studies, providing a holistic view of the current scientific landscape. Insights gleaned from these reviews help refine our understanding of the intricate interplay between gut microbes, inflammation, and gastrointestinal disorders.
In the realm of scientific investigations exploring potential therapies for conditions like IBS and IBD, rigorous methodologies such as double-blind placebo-controlled studies take center stage. These gold-standard trials involve a meticulous design where neither the participants nor the researchers know who is receiving the actual treatment and who is receiving a placebo.
Closing Thoughts
As research continues to unfold, the potential for innovative therapies, such as FMT, and a deeper comprehension of the role of SCFAs, offer hope to patients with irritable bowel syndrome and IBD.
In conclusion, the symbiotic dance between the gut microbes, the immune system, and the enteric nervous system is a captivating journey into the heart of our well-being. As we decode the gut puzzle, the harmony of a balanced microbiome emerges as a key player in fostering digestive health and overall wellness.
At CosmosID, we provide state-of-the-art microbiome sequencing services and bioinformatics tools to support researchers in unraveling this complex microbial tapestry. With our cutting-edge technology, we aim to advance the understanding and treatment of gastrointestinal disorders by decoding the gut microbiome.
Join us on this journey towards a healthier future for all. Contact us today.
Want more like this? Sign-up to our newsletter to get the latest news from CosmosID: